We Specialize in Men's Urological Health Issues
Our Urology specialists offer personalized consultations, treatment plans, and specific procedures to help adult male patients experiencing a variety of urological conditions relating to their urinary or reproductive systems.

There are many urological issues specific to men, can become more common as they age. Urinary health is an important part of men’s overall health. Urology focuses on the health of the urinary tract, which includes the kidneys, bladder, and urethra.
Urologists also study the male reproductive system (testicles, prostate, penis, scrotum, and the tubes that carry sperm) and the problems that could occur. Some common conditions that are found in male urology are enlargement of the prostate, kidney or bladder stones, prostate cancer, bladder cancer, kidney cancer, urinary tract infections, erectile dysfunction, and more.
Our team of specialist urology doctors will discuss any concerns you have about your urinary health. Call us to book an appointment.
Top Reasons Why Men Visit a Urologist
Our experienced staff help many men daily and provide them with clear and concise solutions to their problems. Call us for a confidential and personalized discussion to address your concerns and symptoms or book an appointment.


The Urology Procedures We Offer Men
Our highly-skilled Urological Surgeons are the leading physicians in Cleveland, Athens, and across the Tennessee Valley.
Book an Appointment to discuss your individual needs. Call 423 472-3201
If you are worried about your symptoms talk to us today
Read more about other urological conditions and procedures at:
Many men suffer from urological conditions. It is crucial to understand your health so you can talk about your symptoms and issues with one of our urologists.

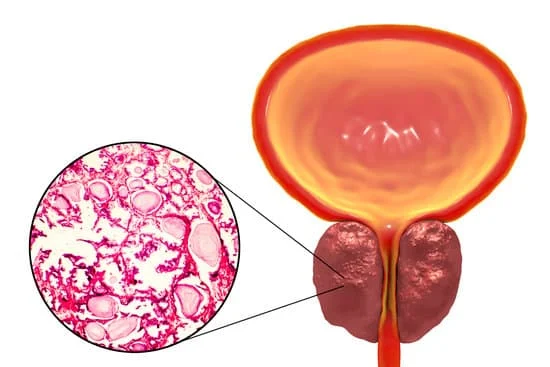
The Male Anatomy
Male urology includes the urinary tract (kidneys, urethra, bladder) and the reproductive organs (testicles, prostate, penis, scrotum, and the vas deferens that carry sperm).
The male urinary tract runs from the kidneys to the bladder to the penis, where urine is excreted. In male reproductive physiology, sperm are made in the testicles. Sperm travel through a tube called the vas deferens and combines with the semen, which is made by the prostate. The semen enters the urethra, which is also used to transport urine.
A urologist specializes in the genitourinary tract and male fertility and is trained for both surgical and medical management of diseases that affect these organs.
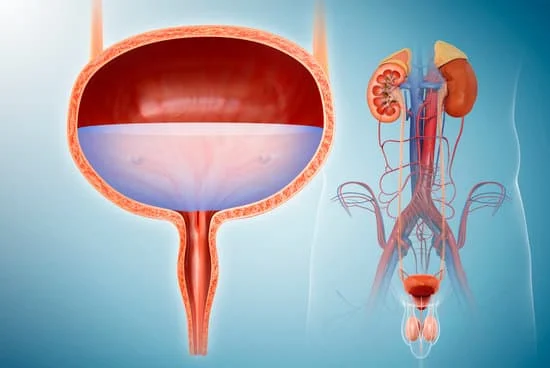
The Urinary Tract
Urine travels through several structures to get where it needs to go. It starts in the kidneys, where it is formed, then passes through two tubes called ureters (one from each kidney) to reach the bladder where it is stored.
When the bladder is full, and you get the urge to pee, it passes through a tube called the urethra to reach the outside via the prostate and penis.
All these structures are together known as the urinary system, and this is what a urologist specializes in.

Early Action on Symptoms
Early detection and prompt treatment are key to better health outcomes.
As the men age, they may experience symptoms of an enlarged prostate, issues with erections, or problems with low testosterone.
If you’re a man experiencing any pain or discomfort, or even a decrease in the urinary stream, or more frequent visits to bathroom at night, contact a urologist promptly. Don’t wait for the symptoms to become worse. Contact us to make an appointment.
Most Common Urology Conditions that Affect Men

One-third of men older than 50, are at risk of BPH
Benign Prostatic Hyperplasia (BPH)
Enlarged Prostate
Benign prostatic hyperplasia (BPH) is caused when the prostate becomes enlarged, putting pressure on your urethra and bladder. Our urologists have helped thousands of men with BPH get back to enjoying life again with a range of available treatments, including lifestyle modifications, medications, minimally invasive procedures, and various surgical options.
You should see one of our doctors if you have trouble going to the bathroom or make trips too frequently. Your doctor can suggest strategies that are right for your particular condition or symptoms. Don’t let this condition stop you from living your best life – call us today!
BPH is NOT Prostate Cancer!
BPH simply means an enlarged prostate. To be diagnosed with BPH or benign prostatic hyperplasia, you need to have both an enlarged prostate and symptoms of a swollen prostate.
How Does the Prostate Work?
The Prostate produces fluid that is about 70% of semen. This may surprise some people as many believe that the testicles produce semen. Testicles only produce the sperm, which travels to the prostate, mixed with the fluid, and ejaculated as semen.
The prostate is located below the bladder. It surrounds the urethra (which carries urine from the bladder to the penis) and the ejaculatory duct (semen from the prostate to the penis).
Although BPH can be slow to develop, you may find that it progresses rapidly. If you experience frequent or urgent urination at least every other day, then it’s likely that you have some degree of BPH.
Lifestyle Changes Can Help
Studies suggest that certain lifestyle changes can prevent some BPH cases. Regular exercise, avoiding alcohol and a low-fat diet that is high in vegetables and protein, including red meat can help you avoid prostate problems, especially if you have a family history.
What are the Symptoms of BPH or Enlarged Prostate?
BPH occurs when the enlarged prostate applies pressure to the tube-like structures that pass through it. Some common symptoms for BPH are:
- Pain and/or difficulty urinating
- Urgent need to urinate or sudden urges during sleep
- Dribbling after you have finished urinating
- A weak stream of urine (you need to be very close to the urinal)
- Frequent urination due to only small amounts each time; hence your bladder is never empty completely
Treatments for BPH or Enlarged Prostate?
Different medications, surgical procedures, diets, and even lifestyles can help during enlarged prostate treatment. Depending on the severity of your condition and BPH symptoms, your doctor may recommend other therapies before trying surgery.
If your condition remains untreated or becomes more severe, your doctor might recommend medications such as alpha-blockers or 5-alpha reductase inhibitors. They may also suggest minimally invasive procedures Urolift or Rezum Treatment.
If these options are not effective and symptoms persist, you may need surgery. Surgery aims to remove excess tissue from your prostate using different techniques such as transurethral resection (TURP), laser-assisted techniques, or ablation methods that destroy tissue by delivering electrical currents. Your doctor will suggest the best treatment plan for your condition.
Elevated PSA Levels - Get Yours Checked!
Elevated prostate-specific antigen (PSA) levels are one of the earliest signs that something might be wrong with your prostate gland. There are several conditions that can cause elevated levels, including benign prostatic hyperplasia (BPH), infection, inflammation, or prostate cancer.
A test with a higher than normal reading doesn’t mean you have prostate cancer—it simply means you need more tests to find out what’s causing it.
What is PSA? What's Abnormal?
Prostate-specific antigen (PSA) is a blood test that primarily screens for prostate cancer. An Elevated PSA is alarming but does not necessarily mean you have cancer. Several other factors can influence your PSA levels.
Normal PSA levels are between 0.4 and 4.0 ng/mL for men aged 20-39. It’s also normal for men aged 40-49 to have levels between 2.5 and 4.0 ng/mL and up to 6.0 ng/mL after age 50.
Your urologist can assess your condition by measuring your PSA levels along with a physical examination and possibly additional tests such as a biopsy or ultrasound.
How Often Should I Check PSA?
PSA is a simple protein produced by prostate cells and detected by blood tests. Regular tests can help you catch prostate cancer early before it spreads. And earlier detection means better treatment outcomes and fewer complications in the long run.
The American Urologic Association recommends men ages 55 to 69 talk with their urologist about annual testing and check-ups. Generally, it is recommended that PSA testing stops at age 75. However, for men over 70, we recommend testing at the discretion of you and your doctor.

How Serious are Raised PSA Levels?
To help determine whether or not a raised PSA is a cause for concern, your doctor will run additional tests such as a biopsy and a physical exam. Be sure to inform your urologist of other symptoms such as UTIs, frequent, painful, or sudden urges to urinate, which could indicate an enlarged prostate.
Peyronie's Disease
Peyronie’s disease refers to the development of scar tissue in the erectile tissue of the penis, which causes the penis to bend or curve during an erection. If you experience pain or inflammation or notice a curve in the penis, consult one of our competent Urologists. They can evaluate and guide the available treatments.
At Tennessee Valley Urology Center, we see patients with Peyronie’s condition regularly. Talk to one of our understanding staff today for assistance in scheduling a consultation.

What is Peyronie's Disease?
Peyronie’s disease is characterized by painless plaques (collagen that has hardened) that develop in the penis. The plaques can cause scar tissue to grow inside the corporal bodies (erectile tissue), sometimes causing penile pain and may alter the shape of the penis while erect and change the rigidity of the erection.
Scar tissue that develops in the penis can cause a bend or curve during erection. It can develop after an injury to the penis or spontaneously. Peyronie’s disease can cause long-term problems if left untreated, so schedule a consultation with one of our urology specialists.
Symptoms of Peyronie's Disease
Although symptoms may vary in each case, men who have Peyronie’s disease usually report symptoms such as:
- A noticeable bend or curve of their penis when they are flaccid or erect
- Penile tenderness
- Painful erections and/or sexual intercourse
- Difficulty achieving orgasm
- A softer than usual erection.
Treatment
Following your consultation, an individualized treatment plan is formed based on the severity of the curve and the degree of erectile dysfunction. The treatment options range from medications to surgical procedures. Call us today to book your appointment for an open discussion with one of our urologists.
Erectile Dysfunction (ED)
Erectile Dysfunction (ED) is a common problem in men over 40. Nearly half of all men will deal with erectile issues at some point in their lives.
Erectile dysfunction can be caused by a range of physical and emotional factors. Uncovering the cause is often a key to finding a solution to this problem and enjoying happy and healthy sex life.
If you have erectile dysfunction, talk to our specialists. We can help you get back to living a healthy and active sex life again.
Symptoms of erectile dysfunction
ED affects up to 30 million men annually in the United States. Some symptoms of this issue are:
- Inability to have an erection
- Reduced sexual desire
- Difficulty in getting an erection
- Trouble achieving orgasm
- Low self-esteem due to ED
It can be hard to diagnose erectile dysfunction yourself. It’s normal for each person to experience symptoms differently, and that’s why it’s important to discuss your concerns and issues with your Urologist.
Our Urology specialists are highly adept in successfully treating men with Erectile Dysfunction, regardless of the cause. If you face any of these symptoms, call us to schedule a consultation with one of our experts.
Physical Causes of ED
A large percentage of ED cases are caused by physical issues such as:
- Diabetes
- Obesity
- High Blood Pressure
- High cholesterol
- Heart Disease
- Vascular disease
- Alcoholism or Substance Abuse
- Physical Injuries to the pelvic area
- Peyronie’s disease
- Use of Tobacco
- Some medications such as
- Anti-hypertensives
- Anti-depressants
- Diuretics
- Beta-blockers
Psychological Causes of ED
- Stress
- Anxiety
- Depression
- Mood Disorders
- Other mental health conditions
Testosterone Deficiency in Men
Testosterone actually plays a role in both men and women. In men, this hormone stimulates sex drive, helps to maintain bone density and muscle development, and supports sperm production.
Causes of Low Testosterone
There are many possible causes of low testosterone. Examples include:
- Obesity
- Diabetes
- Smoking
- Chronic illnesses like heart disease or sleep apnea
- Treatments for other health conditions
- Certain medications like steroids such as prednisone or seizure medications
Signs and Symptoms of Low Testosterone
Low testosterone levels can cause a variety of symptoms. The most common ones include:
- Low sex drive
- Fatigue
- Weight gain
- Low energy
- Difficulty achieving an erection
- Low semen volume
- Loss of muscle mass
- Mood swings
Low Testosterone Treatment
Low testosterone is a common problem that many people face, but it’s curable, and you don’t have to continue suffering.
Testosterone replacement therapy (TRT) is available in several different treatment options, including topical gels, injections, pellets, and oral medications. The benefits of TRT include:
- Increase in your libido
- Decrease in mood swings
- Increase in lean muscle mass
- Restores sleeping patterns
- Helps improve bone density
- Boosts self-confidence
- Improves erectile dysfunction
Talk to your urologist about getting started on TRT today.
Male Infertility
Every year, 1 in 10 men in the U.S is diagnosed with male infertility. Because of the lack of awareness on this topic, men often feel alone in their struggle. However, there are certain steps that these men can take to get on the path to parenthood.
Infertility has long been viewed as a woman’s issue. Still, as more research and information comes to light, it has become increasingly apparent that male infertility can be as common as female infertility. According to National Infertility Association, about one-third of the couples who are struggling with infertility are dealing with male infertility.
What is Male Infertility?
Male infertility is defined as the inability of a man to cause a pregnancy with his sperm.
In couples who have been trying for one year without success, fertility specialists often begin testing for female problems. If the female evaluation is normal, then a male infertility evaluation should be performed.
What is Male Infertility?
Most of these factors are out of your control, but there are a few things you can do to improve your chances at conception. If you want a baby but have trouble conceiving, speak with your doctor about what you can do for low sperm count or other common causes of male infertility.
Risk Factors That Affect Male Fertility
Smoking, obesity, alcohol use, and age are modifiable risk factors that affect male fertility. Other factors affecting male fertility include diabetes, varicocele (when veins in the testicles become enlarged), a sedentary lifestyle, and poor diet.
Regular exercise and eating well will also help prevent other health issues affecting infertility like erectile dysfunction, diabetes, or cardiovascular disease.

What Causes Male Infertility?
A lack of sperm in the semen (Azoospermia) is a common cause for men with fertility problems. Sometimes the sperm is abnormally shaped, which makes fertilization difficult. The common causes of male infertility include:
- Enlarged veins in the scrotum (Varicocele)
- Infections in the reproductive organs
- Hormonal disorders (e.g. Low T)
- Autoimmune or genetic diseases
- Neurological disorders
- Cancer treatments (such as radiation therapy)
- Environmental factors (such as exposure to toxic chemicals)
- Lifestyle factors such as alcohol or smoking
Stop worrying! Take action today!
Talk to us TODAY
and guide you to the best possible solution.
Prostatitis
Prostatitis is the inflammation of the prostate gland. It affects up to 10% of men in their lifetime and is most prevalent in men between the ages of 20-50. The condition can be very mild and cause no symptoms, or it can be painful and severely disrupt a man’s life.
What is Prostatitis?
Prostatitis may be caused by bacteria or it may be due non-bacterial inflammation, such as pelvic floor muscle dysfunction.
Bacterial prostatitis accounts for about 90 percent of all cases. Chronic, long-term forms of prostatitis are rare, but if left untreated, this condition can lead to painful blockage within your prostate that can obstruct urine flow and potentially damage your kidneys. It can also cause chronic pain and infertility in some men.
What are the Symptoms of Prostatitis?
The symptoms of prostatitis are similar to those of other types of urinary tract infections.
Common symptoms include:
- Frequent and painful urination
- Burning sensation during urination
- A strong urge to urinate
- Sometimes blood in the urine
As the condition worsens or is left untreated, it can cause symptoms like:
- Lower back pain that does not go away
- Pain or difficulty having an erection and fatigue
If you experience these symptoms repeatedly over several months, then it’s important that you see your doctor.
What are the Causes of Prostatitis?
There are numerous causes of prostatitis, including bacterial infections and chronic inflammation, which can develop over time, resulting in prostatitis.
The medical community is still unsure why some men develop bacterial prostatitis. Still, certain factors such as autoimmune disease can make you more susceptible to getting an infection in your prostate gland.
Diagnosing Prostatitis
If your doctor suspects that you have prostatitis, you will need a prostate exam.
If you have concerns, talk to your urologist about your options.
Our Renowned Urology Surgeons have Helped Many Men with these Procedures
Below we have provided some more information to help you understand these specific urological procedures for men
The 'No Scalpel' Vasectomy
The No-Scalpel Vasectomy is an effective and safe procedure for men seeking a permanent birth control method. Here’s what you need to know about this procedure.
How is a No Scalpel Vasectomy Done?
Patients are awake for the procedure. A local anesthetic is used to numb the skin, and once it takes effect, your doctor will make a very small puncture in your scrotum to gain access to each vas deferens (the tubes that carry sperm). Each vas deferens is lifted through the puncture.
Your doctor will cut and seal the tubes using cautery or heat. The puncture site is closed with or without a small stitch.
What are the risks of the procedure?
Other than the tiny puncture and a little bit of swelling, you’ll barely be able to tell that you had surgery. You can even go back to work after a few days.
Most men are back to their usual activities within a week or so. You should rest completely for at least two days after the procedure (there are some activities—including sex—that aren’t recommended for at least a week), but there’s no downtime beyond that.
How Should I Prepare For The Procedure?
Before you have a no scalpel vasectomy, your doctor will review potential risks and discuss how to prevent infection after surgery. The scrotum should be shaved and cleaned before the procedure. You may be given medication to take before the procedure to help you relax.
What Should I Anticipate After Surgery?
You will probably have to take a few extra days off work to recover from your no scalpel vasectomy, so make sure you have the time off approved by your employer. You’ll be up and moving around after surgery, but you’ll need time to rest afterwards.
Be aware that you WILL need to use other methods of contraception before your sperm count is confirmed to be zero, which is usually after about 12 weeks. You will still be able to ejaculate semen during sex, the only difference is that it won’t contain sperm.
How long does it take to recover?
After a vasectomy, it’s recommended that you abstain from sex for at least a week. You can get back to normal activities within a few days of the procedure, but resting for the first 48 hours is recommended.
Prostate Ultrasound | Prostate Biopsy
Prostate ultrasound and biopsy can help confirm the presence of prostate cancer or other abnormalities in the prostate. Both procedures are generally safe.
However, as with all medical tests that involve needles or probes being placed inside of your body, there’s always a slight risk that you could have an adverse reaction or infection from these tests. If you do experience any reactions, then your doctor will monitor you closely. If you’re having a biopsy, then you may experience some discomfort due to the needle. The needle used for biopsies is small, but the insertion can still be uncomfortable. Numbing medicine is used to reduce any discomfort.
Here’s what to expect during your procedure so you can be prepared.
What is an Ultrasound?
First of all, ultrasound (or sonogram) is a technology that uses high-frequency sound waves to produce images on a computer.
In medical settings, it’s primarily used for imaging soft tissues like muscles, organs, fat and blood vessels. It is non-invasive and there is no risk of radiation exposure.
How is Prostate Ultrasound performed?
A prostate ultrasound involves using a probe the size of a finger that is inserted into your rectum. Sound waves from the probe will bounce off the prostate and form an image that can be viewed by the urologist. There is minimal pain involved with this test and you can resume normal activities after.
What is a Biopsy?
A biopsy is a procedure during which a sample of tissue is removed from your prostate using ultrasound guidance.
Your doctor will use local anesthesia to numb the prostate area before removing tissue samples from your prostate gland.
During the procedure, a biopsy needle is used to remove several samples from different depths within your prostate in order to get as wide a sampling as possible.
A pathologist then examines these samples under a microscope in search of cancerous cells.
How can you prepare for a biopsy?
To prepare for a biopsy, your doctor will task you to use an enema before the procedure to clean out the rectum. You will also be asked to empty your bladder before the biopsy. The entire procedure takes about 10 minutes when done in the doctor’s office.
You might want to bring a friend or family member to your doctor’s office for support. You might also want to be sure you have someone available to drive you home after, although most patients can drive home without needing someone else.
How long is recovery after a biopsy?
After a biopsy, you will generally require only 48 hours of rest, after which you can resume your normal activities.
You may experience slight pain or discomfort after the procedure, but this is usually mild. It is common to see some blood in the urine, blood in the stool, and blood in the semen. It may take a few days for this to clear up, which is normal.

UroLift® System for Benign Prostatic Hypertrophy
UroLift is an effective treatment for men with symptoms of BPH. UroLift is a minimally invasive procedure that uses implants that hold open the prostate so that the urinary channel is unobstructed to relieve urinary symptoms caused by an enlarged prostate.
Here’s what you need to know about Urolift so you can make an informed decision if it is right for you.
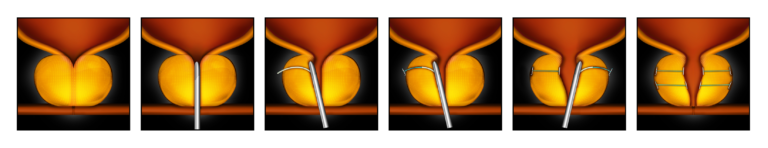
How is UroLift performed?
The Urolift procedure uses a UroLift delivery device which is guided through the urethra using cystoscopy (a method that uses a camera to visualize the bladder).
The implants are placed into the two lobes of the prostate that are compressing on the urethra, which creates an open channel.
By doing this, the part of the urethra (urinary passage tube) that was being blocked because of the prostate is opened. This helps to relieve the symptoms caused by an enlarged prostate.
What are the Benefits?
The Urolift procedure is a proven and effective treatment for symptoms due to an enlarged prostate. Some of the benefits of this procedure include:
- It is minimally invasive with a very quick recovery
- It offers immediate relief of urinary symptoms
- There is rarely a need for a catheter after the procedure
- It preserves ejaculation and sexual function
- No need for ongoing medication
- It is cost-effective and convenient
- There is no hospitalization and patients can go home immediately after the procedure
What are the risks?
This is a generally safe procedure. However, there is a very minimal risk of bleeding, infection, or symptoms of burning or irritation after the procedure.

Introducing the Rezum Prostate Treatment for BPH
If you suffer from Benign Prostatic Hyperplasia (BPH), you’re not alone. This condition is so common that approximately 50% of men over the age of 50 experience symptoms, like frequent urination and weak or interrupted urinary stream.
Fortunately, there are many ways to treat BPH, including medications, lifestyle changes, and minimally invasive surgery. Here, we’ll discuss the latter option – minimally invasive surgery – and introduce you to Rezum, an innovative procedure that’s gaining popularity as an effective BPH treatment.
What Is the Rezum Prostate Treatment for BPH?
Rezum is a minimally invasive procedure that may help men who suffer from benign prostatic hyperplasia. During this procedure, your doctor will use water vapor to heat and shrink prostate tissue, with the goal of improving symptoms over time.
Contact your urology doctor today to learn more about how Rezum can improve your quality of life.
How Does it Work?
Rezum uses steam to decrease the prostate size. It’s a safe procedure that is performed in the office in just 15 minutes. It’s surprisingly effective too, with 80% of men experiencing symptom improvement in a recent clinical study.
The Rezum device is inserted into the urethra through the penis. The device has a retractable needle that is inserted into the prostate so that steam can be injected. The steam is injected in 9-second bursts. Multiple steam injections are performed.
The water vapor causes damage to the prostate cells and these cells are then destroyed by the body. This ultimately results in the prostate shrinking in size and symptom relief.

What to expect before the Rezum procedure
Before you have this treatment, you will need to undergo an assessment period. This will involve a thorough interview with your doctor as well as a physical examination which includes a digital rectal examination. There are other tests that are done. A cystoscopy is performed, where a small camera is inserted into the penis to look at the prostate and bladder. A prostate ultrasound is also used at times to measure prostate size.
All of this is done in order to get a complete picture of your overall health and your prostate. Before the procedure, you may need to start taking antibiotics to prevent infection after the procedure.
What to expect after the Rezum procedure
The Rezum prostate treatment for BHP is quick and takes less than 15 minutes. Afterward, most men resume normal activities within a few days. Men will wear a catheter for 2-3 days after the procedure. This is placed in your bladder through your penis. It is necessary because the prostate can swell after the procedure, which may affect urine flow.
Some men may need to take some time off from work after the procedure, but generally your daily activities will not be affected. Most importantly, many men experience significantly improved urinary flow and reduced prostate size after undergoing this procedure.
When the catheter is removed, you should gradually notice an improvement in your urine flow and other urine symptoms. Some men may have increased urgency – the sudden and compelling need to urinate – in the initial few weeks after the procedure but this generally improves with time.
Be Confident in the Quality of Advice at Tennessee Valley Urology
A Guide to Testopel Insertion
(Testosterone Replacement Therapy)
Testosterone Replacement Therapy (TRT) is used to treat men who have low testosterone levels. It is an effective and safe way of increasing your testosterone to normal levels, allowing you to get your life back!
One method of TRT is the Testopel implant, which is an FDA-approved brand of subcutaneous testosterone pellets. These pellets are an effective way to increase testosterone levels in men who have low testosterone.
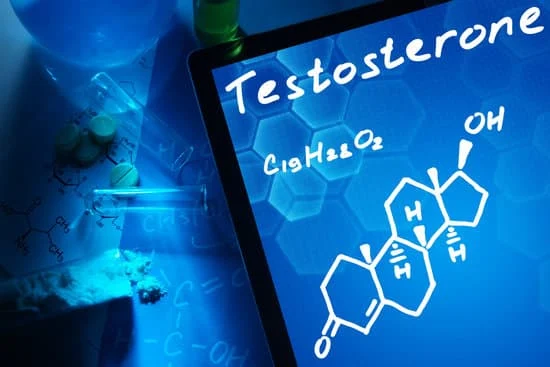
What is Testopel?
Testopel is a form of injectable testosterone replacement therapy (TRT) in which pellets containing testosterone are inserted under your skin.
The pellets help to restore normal levels of testosterone. This method has been shown to be an effective method for many patients.
How is Testopel administered?
It’s a really simple procedure which involves a treatment every 3 to 6 months.
The treatment is done in the doctor’s office and takes less than 10 minutes.
During the procedure, your doctor will numb a small area in the skin in the buttock area with injection of local anesthesia. A small incision is made and then the pellets are inserted just under the skin.
These pellets slowly release testosterone into the body over an extended period of time without the need for weekly injections or daily gel applications. The pellets dissolve slowly and last up to 3-6 months.
Risks and Side Effects
As with all medications, there are side effects that come with testosterone replacement therapy. With testopel, there can be irritation at the injection site. Infection is rare but can happen. Testosterone can increase the blood to become too thick or viscous, so it is important to monitor your blood levels while on this treatment.
There are also several potential side effects to testosterone replacement including:
- Acne
- Body hair growth
- Oily skin
- Prostate enlargement
- Infertility
- Infection at the implantation site
If you experience any of these, talk to your urologist about alternative treatment options.
Penile Injection Therapy
Penile injection therapy involves injecting medication directly into the penis to treat erectile dysfunction (ED). They treat the situation by allowing better blood flow to the penis.
A trimix of medicine: alprostadil, phentolamine, and papaverine is injected into the penis. The Injection causes an erection in about 80% of men with ED.
Penile injection therapy, more commonly known as penile injections, is a minimally invasive procedure that helps men with erectile dysfunction by causing an erection through medication injected directly into the penis.
The smooth muscle relaxers help increase blood flow to the penis by relaxing blood vessels, allowing blood to flow freely.
How does it work?
After numbing your penis with a local anesthetic, your doctor will inject one or two drug compounds directly into your penis using a very fine needle.
These compounds may increase blood flow to help you get and keep an erection, or they may relax certain muscles in your penis to produce erections on their own.
It’s also possible that a combination of drugs may be used in certain situations. According to experts, penile injection therapy treats impotence in about 90 percent of men who try it, making it more effective than oral medication and less invasive than most other treatments.
The erections will generally last between 30 to 60 minutes. An injection is given directly into a particular part of your penis during a 10- to 15-minute procedure.
Who can use this treatment?
Urological injection therapy is reserved primarily for men with erectile dysfunction, and it is mainly second-line treatment when oral medications have failed.
Also, some men may experience some side effects associated with taking oral medications and would prefer injections instead.
Don’t consider it an option until you’ve tried all other forms of treatment. That said, if none of these alternatives have worked, a penile injection may be worth considering as a last resort.
Are there any side effects?
Although a safe procedure under a qualified urologist, some side effects with penile injection therapy are:
- Priapism (painful erections lasting more than four hours)
- Hematoma (blood-filled swelling)
- Fibrosis and/or injection granulomas (non-cancerous lumps at the injection site)
Annual Check-ups - Stay Healthy in Your Golden Years
If you are aged 50 years or above, it’s time to start yearly check-ups to maintain good urological health. Most men can manage any urological conditions without invasive treatments if their condition is diagnosed early and treated quickly.
Your annual urology check-ups will assess the critical organs in your urinary system – kidneys, urethra, bladder, prostate, and penis to ensure they are all functioning as expected. It is usually a combination of a physical examination and blood and urine samples. Your doctor may prescribe additional tests depending on your symptoms.
Screening for Prostate Cancer
In general, screening for prostate cancer isn’t recommended for men under 50.
That said, you can find out your baseline PSA levels by taking a free blood test through your primary care physician at age 40 or 45.
If that number is higher than normal, you may want to get more tests, including an MRI and biopsy.
If you have an immediate family history of prostate cancer (or a personal history of breast cancer), talk with your doctor about whether routine testing is right for you at a younger age.

Benefits of Regular Check-Ups
Screening can help find prostate cancer early when it’s easier to treat. It can also reduce the risk of dying from prostate cancer.
According to some studies, screening men older than 50 who are at average risk for prostate cancer may help save lives.
These studies have shown that among those who undergo routine screening, fewer die of prostate cancer over a period of 10 years.
If you’re diagnosed with aggressive or advanced prostate cancer, you may have better treatment options when it’s found early.
Treatment options are often limited when the disease is detected later.
Doctors recommend annual screenings if you’re above 50—especially if you have additional risks such as a family history of prostate cancer or African-American heritage. They are more likely to develop aggressive forms of prostate cancer.
That said, not getting tested leaves you open to having an undetected prostate tumor grow into an advanced stage while increasing your chances of death from prostate cancer — so discuss what’s right for you with your urologist.
Guidelines on when and how often you should be screened may vary slightly depending on where you live.
Prevention is Better than a Cure
Just because you’re over 50 doesn’t mean your doctor visits are any less important. In fact, some checkups can only be done by your primary care physician or a specialist after certain milestones, like 50.
The good news is that when you take good care of yourself and stay up-to-date on routine health screenings, you’ll live a long life full of quality years.
And when it comes to your annual physicals: never skip one—even if you’re feeling fine—because it could be more than just an annual doctor visit—it could be early detection for cancer or another disease.
Skip these tests and you might put yourself at risk later down the road. So make sure to schedule all your yearly visits with your primary care physician; doing so will ensure you have all bases covered in order to live a healthy and happy old age.
It’s never too early or too late to be proactive about your health.

Male Circumcision
Male circumcision is a surgical procedure that removes the foreskin (the skin covering and protecting the penis). Aside from religious or cultural reasons, a circumcision is commonly done in adult men to treat conditions like phimosis (the inability to retract the foreskin), swollen foreskin, or inflammation of the tip of the penis.
In newborn boys, circumcision is typically performed within days of birth, but it can be done at any age.

How is it performed?
For adult patients, the procedure is done under anesthesia. The foreskin is carefully removed. The skin that remains is brought back together and sutured with a dissolvable stitch. These stitches will go away on their own and do not need to be removed in the office. A dressing is then placed over the penis.
The Benefits of a Circumcision
There are many benefits to having circumcision. The most notable benefits are:
- A decreased risk of contracting and spreading sexually transmitted diseases, though protection is still essential
- It will be easier to maintain good genital hygiene
- Reduced risk of penile cancer
- Prevention of penile diseases such as phimosis (being unable to retract the foreskin) or paraphimosis (returning it after it’s been retracted)
Risks Associated With Circumcision
There are very few risks associated with male circumcision. The most common complications are bleeding and infection. However, this is fairly rare. Most bleeding is mild and requires no treatment. However, in some cases it can occasionally lead to hematoma or excessive blood loss if left untreated.
How to prepare for the procedure
Before you’re circumcised, your doctor will perform a pre-op assessment to check for any underlying conditions that may affect the operation. They will direct you to avoid taking drugs like Aspirin before the surgery as well, as this may cause excessive bleeding.
A circumcision is an outpatient procedure, so you will not be admitted and you can go home soon after it’s done.
What to expect after the procedure
After a circumcision procedure, you will need to go home and rest. To minimize swelling and discomfort, you can take an over-the-counter pain reliever (such as ibuprofen). However, you should avoid taking aspirin or any other medication that contains aspirin if possible. You can also use ice packs to help relieve swelling.
Be sure to follow your doctor’s instructions regarding after care. You should stay away from harsh chemicals like alcohol that dry out the skin.

Speak to one of our Urology Experts for Caring and Dependable Advice
TVUC ~ Proudly Helping Men in our Communities with their Urological Health
You can rely on the expert and competent care you will receive from the Tennessee Valley Urology Team at our Cleveland and Athens offices. Call us today to book your appointment to discuss your symptoms and get results – FAST!
Treating Patients in Cleveland TN and the surrounding towns
- Benton
- Hopewell
- McDonald
- Ocoee
- Ooltewah
- Reliance
- Snow Hill
- South Cleveland
- Wildwood Lake
Helping Patients in Athens TN and the the surrounding towns
- Decatur
- Etowah
- Madisonville
- Niota
- Riceville
- Sweetwater
- Williamsburg
Supporting Patients around Copper Basin, Georgia GA, North Carolina NC
- Ducktown
- Harbuck
- Wildwater
- Blue Ridge
- Mccaysville
- Murphy
